Sidoinnehåll
Kärlaccess – Angio och PCI via arteria radialas eller femoralis
Läs om kärlocklusionssystem på följande sidor: TR-band, femostop.
Historiskt sett (se avsnitt om historisk utveckling nedan) har arteria femoralis i många år varit standardaccess för PCI, men idag används arteria radialis i Sverige i 85 % av fallen för PCI och koronarangiografi (se SWEDEHEART registret). Oftast används höger radialisartär, för att PCI-operatören står på patientens högra sida, man kommer då lättare åt högerarmen. Vänstra radialis används huvudsakligen för CABG-opererade patienter som har fått ett LIMA-graft (enkelt att komma åt via vänster radialas, LIMA avgår från vänstra a subclavia) eller om höger radialas är ockluderad, till exempel efter tidigare punktion. Arteria femoralis används idag för mer komplexa ingrepp som kräver större katetrar (CTO, vissa bifurkartioner, klaffingrepp), patienter i chock när radialispuls saknas, en del av “gammal vana” eller för CABG-opererade patienter när operatören inte vill använda vänstra radialis. Kort sammanfattat är femoralis-stick enklare, ger ofta bättre stöd men har större risker.
Videos
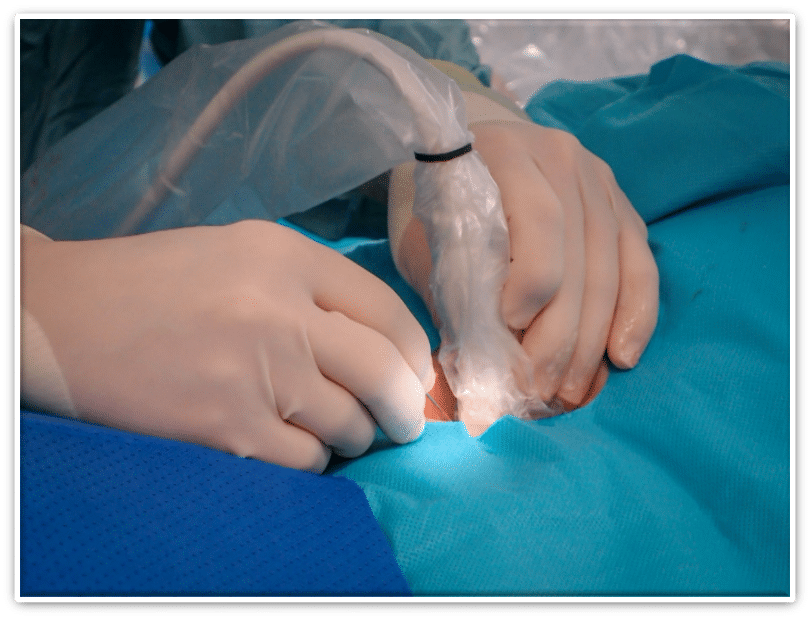
Radialispunktion
Femoralispunktion
Angioseal
Angio-Seal är ett system som implanterar ett ankare på kärlets insida och fäster den via en suturtråd på en kollagenplugg som ligger på kärlets utsida, en s.k. „sandwich system“. Systemet resorberas inom 90 dagar. Finns i 6F och 8F.
Sammanfattning för- och nackdelar
ARTERIA RADIALIS:
- fördelar:
- Ingen relevant blödningsrisk
- Patienten kan mobiliseras direkt efter ingreppet
- Patienten slipper bli steriltvättad i ljumsken med flera personer i rummet
- nackdelar:
- Begränsning till mindre kateterdiameter (7F hos män, ofta mindre hos kvinnor)
- Vänster radialis: Kräver ibland en för operatören ansträngande kroppshållning (ryggvärk!)
- Små diametrar hos mindre kvinnor
- Risk för smärtsam kärlspasm (bästa profylax är god sedering)
- Olämplig för patienter som är motoriskt oroliga (svårt att kontrollera armen om patienten vill lyfta den)
ARTERIA FEMORALIS:
- fördelar:
- Större kateterdiameter passar
- Enklare åtkomst vid chock
- Ger ofta bättre kateterstöd än radialis
- Enklare att hitta alla grafter hos CABG opererade
- nackdelar:
- Betydligt större blödningsrisk
- Kräver (enligt vår uppfattning) kärl-ultraljud (för att minska blödningsrisken)
- Patienten behöver ligga plant i ett par timmar efter ingreppet
- Högre kostnad pga ocklusion device som används för att försluta efteråt
Risker/Komplikationer: se “Risker och komplikationer vid koronarangiografi/PCI“
Historisk utveckling av kärlpunktion för angio och PCI:
(originalpublikationen- en disputation från 2019 – är på engelska):
While the history of cardiac catheterization began with access in the arm, the annals of PCI start with access in the groin: In the first catheterization of the human heart in a living person, Forssman conducted a self-experiment in 19291 in the form of an antecubital venesection for vascular access. The first selective human coronary catheterization, unintentionally performed by Mason Sones on a patient slated for aortography in 1958,2 was likewise achieved via the arteria brachialis. Later, after the Seldinger technique was developed in Sweden in the 1950s3 and became more widely known in the 1960s, Judkins introduced2 Seldinger access via the arteria femoralis, thus averting the need for surgical cutdown for vascular access. Femoral access (FA) later became the default method for coronary angiography and intervention. So, since the introduction of PCI in 1977, the traditional approach has been the femoral artery45
In 1989, Campeau reported conducting 100 coronary angiographies using the distal radial artery with 5F catheters. In 1992, Ferdinand Kiemeneij, who experienced severe problems with femoral bleeding in heavily anticoagulated patients scheduled for stenting with a Palmaz-Schatz stent, saw the possibility to reduce bleeding and experimented with and then published on PCI that utilized the radial access (RA) technique.6 It then took time for transradial PCI to become more widely used in the 21stcentury.
Since FA was associated with vascular access site complications causing bleeding, ischemia, anddeath,78910 the initial intention of the investigation into the feasibility of RA in clinical practicewas to reduce access-site-related bleeding. This hope for a reduction in access-site complications and a resulting reduction in bleeding is still the main intention of interventional cardiologists who use the more technically demanding RA.
The patient or medical personnel usually notice subcutaneous bleeding from the radial artery after only a few milliliters and treatment by local compression is mostly easy. In-hospital subcutaneous bleeding from the radial artery can, in sporadic cases, lead to compartment syndrome,11 but is highly improbable to cause hemorrhagic shock. In contrast, in-hospital bleeding from a FA site can be difficult to detect, difficult to treat, and can present with hemorrhagic shock as a first symptom.
Other advantages of RA include direct ambulation12 (bed rest is mandatory after femoral puncture),13 resulting in earlier or same-day discharge in stable patients same-day 141, 142 141516 and higher patient satisfaction: Fifty percent of RIVAL patients randomized to FA and 90% of those in the RA group would choose RA for their next procedure.17
A disadvantage of the radial puncture, compared to FA, is the limit in the catheter lumen-diameter (specific interventions have to be carried out with FA for this reason) and the higher technical difficulty of vessel puncture and catheter advancement (due to the minor vessel size and arterial spasm)1819 that are evident mainly at the beginning of an operator’s learning curve,20 but also for experienced operators in cases of anatomical variations (high radial bifurcation, tortuosity, loops).14 The main risk of RA is, mostly asymptomatically, radial artery occlusion,1421 with critical distal ischemia being extremely rare, and minor bleeding, which in rare cases can cause compartment syndrome. Pseudoaneurysmata and fistulae in the radial artery are rare complications: In RIVAL,17 0.2% of patients randomized to RA had an arterial pseudoaneurysm needing closure, compared to 0.4% in the femoral group. To my knowledge, there is no published case of a lethal local complication after RA. It then took more than two decades to gather scientific evidence to prove the initial clinical hypothesis, namely that RA reduces bleeding.
In the first decade of the 21st century, two meta-analyses of several smaller RCTs, published before the larger RCT cited below, showed a reduction in the clinical, significant access-site bleeding by RA.2223 Access-site bleeding, mainly stemming from FA, accounted for 30 to 50% of all bleeding complications in a large study from 2011 (only 8% RA in these patients),24 i.e., the improvement of arterial access can influence a large fraction of bleeding complications. One crucial component of this development was the refinement of operator skills, equipment, closure devices, and anticoagulation strategies in performing FA PCI over time.
In an analysis of 17,900 patients treated with trans-femoral PCI between 1994 and 2005 at the Mayo Clinic,7 major bleeding decreased over time from 8.4 to 3.5% from first to last tertial and retroperitoneal bleeding decreased from 0.8 to 0.3%. The HR for 30-day mortality, adjusted for baseline and procedural characteristics, was 12.8 for major femoral hematoma and 43.8 for retroperitoneal bleeding.
However, the hypothesis that RA could even further reduce bleeding lived on and since 2011, the interventional community has performed several large RCTs to examine this hypothesis. The first large RCT testing the benefit of RA over FA was the RIVAL study, 17 which included 7,021 patients with ACS, non-STE-ACS and STEMI, who were analysed in 2011 by intention-to-treat and showed no difference in the composite primary endpoint (death, stroke, MI, non-CABG bleeding at 30 days) or in the secondary endpoint death at 30 days.
But a pre-specified subgroup analysis showed a significant reduction in the primary endpoint in the 1,958 patients STEMI patients included in RIVAL, as well as in the subgroup of centers in the highest tertial of radial volume (mean >146 radial PCI per operator per year). So, one conclusion derived from RIVAL was that a higher RA rate decreases radial complications, but caution is needed in that a very high operator RA rate might lead to more complications in the cases mandating FA, as the operator might lose FA expertise.25
Concerning bleeding, RIVAL found no significant difference in non-CABG-related major bleeding (access-site-related and non-access-site-related) or in access-site-related major bleeding (0.2% in RA group, 0.3% in FA group, n.s.). Interestingly, in a post-hoc analysis that took the actual bleeding site into account, there were no major access-site bleeds from RA at all compared to 18 major bleeds at the FA point (because of cross-over, subsequent procedures after the index procedure, or femoral IABP insertion.)26
In 2012, the next radial study focused on STEMI patients. The multicenter RIFLE–STEACS 27 study randomized 1,001 patients with STEMI to RA versus FA in four high-volume centers and found a significant reduction in the primary composite endpoint (cardiac death, stroke, MI, TLR, and bleeding) as well as a statistically significant decrease from 9.2 to 5.2% in the 30-day cardiac mortality rate (in the secondary endpoint).
In 2015, the largest vascular access study, the MATRIX study, Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management trial,28 was published: Seventy-eight European centers had randomized 8,404 patients with acute coronary syndromes, non-STE-ACS, and STEMI to RA or FA. The first of the two co-primary endpoints, MACE (death, MI, stroke), was negative (p = 0.03 at a co-primary alpha 0,025), while the second, NACE (net adverse clinical events, defined as MACE plus non-CABG BARC123 major bleeding), was statistically significant (p 0.0092) and clinically significant (RR 0.83, 95% CI 0.73–0.96), driven by a reduction in bleeding and all-cause mortality, with the latter being statistically significant as a predefined secondary endpoint (all-cause mortality 1.6% vs. 2.2%, RR 0.72, 95% CI 0.53–0.99; p = 0.045). The secondary endpoints were all components of the co-primary endpoints, plus cardiovascular mortality and ST, and significance was defined with a two-sided alpha of 5%, i.e., there was no adjustment for multiple comparisons.
In 2016, a meta-analysis including 24 RCTs with more than 22,000 patients concluded that RA, compared to FA, reduced all-cause mortality with an OR of 0.71 (95% CI 0.59, 0.87) and a number needed to treat to benefit (NNTB) of 160, MACE with an OR of 0.84 (CI 0.75, 0.94) and a NNTB of 99, major bleeding by a NNTB of 103, and major vascular complications by more than four-fold, with an OR of 0.25 (CI 0.16–0.35) and a NNTB of 117. 29
Accordingly, a Cochrane review concluded in 2018 that a “transradial approach for diagnostic CA or PCI (or both) in CAD might reduce short-term NACE, cardiac death, all-cause mortality, bleeding, and access-site complications.”30
In summary, these trials provided evidence that when utilized by experienced operators, RA for coronary angiography reduced clinical endpoints as well as all-cause mortality.27 3117 In many countries, as in Sweden, radial puncture has, in recent years, evolved as the primary access strategy for coronary angiography and PCI, but large variations between operators, hospitals, and countries still exist.143233 Based on this evidence, the current 2018 ESC guideline on the management of patients with STEMI includes a strong recommendation for RA.34
However, despite all the evidence in favor of RA, there is an ongoing controversy.35 The external validity of the strong evidence for the impact of RA on mortality from the MATRIX study has been questioned 36 and femoral puncture is still the default strategy for the majority of U.S. operators,37 while there is no recommendation for RA in the U.S. STEMI guideline.38
Litteratur
Contemporary Arterial Access in the Cardiac Catheterization Laboratory (Jacc Cardiovasc Interv 2017)39
Relaterade sidor
Last Updated on July 4, 2024 by Christian Dworeck
- Ny sida: PCI vid förkalkade kranskärl – teknik, tips och evidens - May 6, 2025
- När ska vi gå till akut koronarangio efter hjärtstopp? Ny sida på kardiologi.se - April 16, 2025
- Föreläsning om MINOCA - January 26, 2025
- Meyer JA. Werner Forssmann and catheterization of the heart, 1929. The Annals of thoracic surgery. 1990;49:497-9 [↩]
- Bruschke AV, Sheldon WC, Shirey EK and Proudfit WL. A half century of selective coronary arteriography. Journal of the American College of Cardiology. 2009;54:2139-44 [↩] [↩]
- Seldinger SI. Catheter replacement of the needle in percutaneous arteriography. A new technique. Acta radiologica Supplement. 1952;434:47-52 [↩]
- Gruntzig AR, Senning A and Siegenthaler WE. Nonoperative dilatation of coronary-artery stenosis: percutaneous transluminal coronary angioplasty. The New England journal of medicine. 1979;301:61-8 [↩]
- Barton M, Gruntzig J, Husmann M and Rosch J. Balloon Angioplasty – The Legacy of Andreas Gruntzig, M.D. (1939-1985). Frontiers in cardiovascular medicine. 2014;1:15 [↩]
- Kiemeneij F and Laarman GJ. Percutaneous transradial artery approach for coronary stent implantation. Catheterization and cardiovascular diagnosis. 1993;30:173-8 [↩]
- Doyle BJ, Ting HH, Bell MR, Lennon RJ, Mathew V, Singh M, Holmes DR and Rihal CS. Major femoral bleeding complications after percutaneous coronary intervention: incidence, predictors, and impact on long-term survival among 17,901 patients treated at the Mayo Clinic from 1994 to 2005. JACC Cardiovasc Interv. 2008;1:202-9 [↩] [↩]
- Azzalini L, Tosin K, Chabot-Blanchet M, Avram R, Ly HQ, Gaudet B, Gallo R, Doucet S, Tanguay JF, Ibrahim R, Gregoire JC, Crepeau J, Bonan R, de Guise P, Nosair M, Dorval JF, Gosselin G, L’Allier PL, Guertin MC, Asgar AW and Jolicoeur EM. The Benefits Conferred by Radial Access for Cardiac Catheterization Are Offset by a Paradoxical Increase in the Rate of Vascular Access Site Complications With Femoral Access: The Campeau Radial Paradox. JACC Cardiovasc Interv. 2015;8:1854-64 [↩]
- Johnson LW, Lozner EC, Johnson S, Krone R, Pichard AD, Vetrovec GW and Noto TJ. Coronary arteriography 1984–1987: A report of the registry of the society for cardiac angiography and interventions. I. Results and complications. Catheterization and cardiovascular diagnosis. 1989;17:5-10 [↩]
- Eisen A, Kornowski R, Vaduganathan M, Lev E, Vaknin-Assa H, Bental T, Orvin K, Brosh D, Rechavia E, Battler A and Assali A. Retroperitoneal bleeding after cardiac catheterization: a 7-year descriptive single-center experience. Cardiology. 2013;125:217-22 [↩]
- Tizon-Marcos H and Barbeau GR. Incidence of compartment syndrome of the arm in a large series of transradial approach for coronary procedures. Journal of interventional cardiology. 2008;21:380-4 [↩]
- Wiper A, Kumar S, MacDonald J and Roberts DH. Day case transradial coronary angioplasty: a four-year single-center experience. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 2006;68:549-53 [↩]
- Bangalore S and Bhatt DL. Femoral arterial access and closure. Circulation. 2011;124:e147-56 [↩]
- Hamon M, Pristipino C, Di Mario C, Nolan J, Ludwig J, Tubaro M, Sabate M, Mauri-Ferre J, Huber K, Niemela K, Haude M, Wijns W, Dudek D, Fajadet J, Kiemeneij F, European Association of Percutaneous Cardiovascular I, Working Group on Acute Cardiac Care of the European Society of C and Working Group on Thrombosis on the European Society of C. Consensus document on the radial approach in percutaneous cardiovascular interventions: position paper by the European Association of Percutaneous Cardiovascular Interventions and Working Groups on Acute Cardiac Care** and Thrombosis of the European Society of Cardiology. EuroIntervention : journal of EuroPCR in collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 2013;8:1242-51 [↩] [↩] [↩] [↩]
- Bertrand OF, De Larochelliere R, Rodes-Cabau J, Proulx G, Gleeton O, Nguyen CM, Dery JP, Barbeau G, Noel B, Larose E, Poirier P and Roy L. A randomized study comparing same-day home discharge and abciximab bolus only to overnight hospitalization and abciximab bolus and infusion after transradial coronary stent implantation. Circulation. 2006;114:2636-43 [↩]
- Ziakas AA, Klinke BP, Mildenberger CR, Fretz DE, Williams EM, Kinloch FR and Hilton j GJ. Safety of same-day-discharge radial percutaneous coronary intervention: a retrospective study. Am Heart J. 2003;146:699-704 [↩]
- Jolly SS, Yusuf S, Cairns J, Niemelä K, Xavier D, Widimsky P, Budaj A, Niemelä M, Valentin V, Lewis BS, Avezum A, Steg PG, Rao SV, Gao P, Afzal R, Joyner CD, Chrolavicius S and Mehta SR. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. The Lancet. 2011;377:1409-1420 [↩] [↩] [↩] [↩]
- Pristipino C, Roncella A, Trani C, Nazzaro MS, Berni A, Di Sciascio G, Sciahbasi A, Musaro SD, Mazzarotto P, Gioffre G and Speciale G. Identifying factors that predict the choice and success rate of radial artery catheterisation in contemporary real world cardiology practice: a sub-analysis of the PREVAIL study data. EuroIntervention : journal of EuroPCR in collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 2010;6:240-6 [↩]
- Kiemeneij F, Vajifdar BU, Eccleshall SC, Laarman G, Slagboom T and van der Wieken R. Evaluation of a spasmolytic cocktail to prevent radial artery spasm during coronary procedures. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 2003;58:281-4 [↩]
- Ball WT, Sharieff W, Jolly SS, Hong T, Kutryk MJ, Graham JJ, Fam NP, Chisholm RJ and Cheema AN. Characterization of operator learning curve for transradial coronary interventions. Circ Cardiovasc Interv. 2011;4:336-41 [↩]
- Kotowycz MA and Dzavik V. Radial artery patency after transradial catheterization. Circ Cardiovasc Interv. 2012;5:127-33 [↩]
- Jolly SS, Amlani S, Hamon M, Yusuf S and Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am Heart J. 2009;157:132-40 [↩]
- Agostoni P, Biondi-Zoccai GG, de Benedictis ML, Rigattieri S, Turri M, Anselmi M, Vassanelli C, Zardini P, Louvard Y and Hamon M. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures; Systematic overview and meta-analysis of randomized trials. Journal of the American College of Cardiology. 2004;44:349-56 [↩]
- Verheugt FW, Steinhubl SR, Hamon M, Darius H, Steg PG, Valgimigli M, Marso SP, Rao SV, Gershlick AH, Lincoff AM, Mehran R and Stone GW. Incidence, prognostic impact, and influence of antithrombotic therapy on access and nonaccess site bleeding in percutaneous coronary intervention. JACC Cardiovasc Interv. 2011;4:191-7 [↩]
- Azzalini L, Tosin K, Chabot-Blanchet M, Avram R, Ly HQ, Gaudet B, Gallo R, Doucet S, Tanguay JF, Ibrahim R, Gregoire JC, Crepeau J, Bonan R, de Guise P, Nosair M, Dorval JF, Gosselin G, L’Allier PL, Guertin MC, Asgar AW and Jolicoeur EM. The Benefits Conferred by Radial Access for Cardiac Catheterization Are Offset by a Paradoxical Increase in the Rate of Vascular Access Site Complications With Femoral Access: The Campeau Radial Paradox. JACC Cardiovasc Interv. 2015;8:1854-64 [↩]
- Jolly SS, Yusuf S, Cairns J, Niemelä K, Xavier D, Widimsky P, Budaj A, Niemelä M, Valentin V, Lewis BS, Avezum A, Steg PG, Rao SV, Gao P, Afzal R, Joyner CD, Chrolavicius S and Mehta SR. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. The Lancet. 2011;377:1409-1420 [↩]
- Romagnoli E, Biondi-Zoccai G, Sciahbasi A, Politi L, Rigattieri S, Pendenza G, Summaria F, Patrizi R, Borghi A, Di Russo C, Moretti C, Agostoni P, Loschiavo P, Lioy E, Sheiban I and Sangiorgi G. Radial versus femoral randomized investigation in ST-segment elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. Journal of the American College of Cardiology. 2012;60:2481-9 [↩] [↩]
- Valgimigli M, Gagnor A, Calabró P, Frigoli E, Leonardi S, Zaro T, Rubartelli P, Briguori C, Andò G, Repetto A, Limbruno U, Cortese B, Sganzerla P, Lupi A, Galli M, Colangelo S, Ierna S, Ausiello A, Presbitero P, Sardella G, Varbella F, Esposito G, Santarelli A, Tresoldi S, Nazzaro M, Zingarelli A, de Cesare N, Rigattieri S, Tosi P, Palmieri C, Brugaletta S, Rao SV, Heg D, Rothenbühler M, Vranckx P and Jüni P. Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management: a randomised multicentre trial. The Lancet. 2015;385:2465-2476 [↩]
- Ferrante G, Rao SV, Juni P, Da Costa BR, Reimers B, Condorelli G, Anzuini A, Jolly SS, Bertrand OF, Krucoff MW, Windecker S and Valgimigli M. Radial Versus Femoral Access for Coronary Interventions Across the Entire Spectrum of Patients With Coronary Artery Disease: A Meta-Analysis of Randomized Trials. JACC Cardiovasc Interv. 2016;9:1419-34 [↩]
- Kolkailah AA, Alreshq RS, Muhammed AM, Zahran ME, Anas El-Wegoud M and Nabhan AF. Transradial versus transfemoral approach for diagnostic coronary angiography and percutaneous coronary intervention in people with coronary artery disease. The Cochrane database of systematic reviews. 2018;4:Cd012318 [↩]
- Valgimigli M, Gagnor A, Calabró P, Frigoli E, Leonardi S, Zaro T, Rubartelli P, Briguori C, Andò G, Repetto A, Limbruno U, Cortese B, Sganzerla P, Lupi A, Galli M, Colangelo S, Ierna S, Ausiello A, Presbitero P, Sardella G, Varbella F, Esposito G, Santarelli A, Tresoldi S, Nazzaro M, Zingarelli A, de Cesare N, Rigattieri S, Tosi P, Palmieri C, Brugaletta S, Rao SV, Heg D, Rothenbühler M, Vranckx P and Jüni P. Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management: a randomised multicentre trial. The Lancet. 2015;385:2465-2476 [↩]
- Mamas MA, Nolan J, de Belder MA, Zaman A, Kinnaird T, Curzen N, Kwok CS, Buchan I, Ludman P, Kontopantelis E, British Cardiovascular Intervention S and the National Institute for Clinical Outcomes R. Changes in Arterial Access Site and Association With Mortality in the United Kingdom: Observations From a National Percutaneous Coronary Intervention Database. Circulation. 2016;133:1655-67 [↩]
- Anderson HV. Transradial Access for Primary Percutaneous Coronary Intervention: Catching On and Catching Up. JACC Cardiovasc Interv. 2017;10:2255-2257.162. Eleid MF, Rihal CS, Gulati R and Bell MR. Systematic use of transradial PCI in patients with ST-segment elevation myocardial infarction: a call to “arms”. JACC Cardiovasc Interv. 2013;6:1145-8 [↩]
- banez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimsky P and Group ESCSD. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). European heart journal. 2018;39:119-177 [↩]
- Eleid MF, Rihal CS, Gulati R and Bell MR. Systematic use of transradial PCI in patients with ST-segment elevation myocardial infarction: a call to “arms”. JACC Cardiovasc Interv. 2013;6:1145-8 [↩]
- Shah R and Ahmed AJ. Validity of Randomized Trials Comparing Radial Versus Femoral Access in Acute Coronary Syndrome. JACC Cardiovasc Interv. 2016;9:1517-8 [↩]
- Valle JA, Kaltenbach LA, Bradley SM, Yeh RW, Rao SV, Gurm HS, Armstrong EJ, Messenger JC and Waldo SW. Variation in the Adoption of Transradial Access for ST-Segment Elevation Myocardial Infarction: Insights From the NCDR CathPCI Registry. JACC Cardiovasc Interv. 2017;10:2242-2254 [↩]
- O’Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr., Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW and American College of Cardiology Foundation/American Heart Association Task Force on Practice G. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:e362-425 [↩]
- Sandoval Y, Burke MN, Lobo AS, Lips DL, Seto AH, Chavez I, Sorajja P, Abu-Fadel MS, Wang Y, Poulouse A, Gössl M, Mooney M, Traverse J, Tierney D, Brilakis ES. Contemporary Arterial Access in the Cardiac Catheterization Laboratory. JACC Cardiovasc Interv. 2017 Nov 27;10(22):2233-2241. doi: 10.1016/j.jcin.2017.08.058. PMID: 29169493. [↩]

